Overcoming Overuse Injuries: A Guide to Prevention and Healing
In today’s fast-paced world, many of us lead active lives and engage in various physical activities. While being active provides numerous health benefits, it can also lead to overuse injuries. Overuse injuries occur when repetitive movements put excessive stress on specific parts of the body, resulting in pain and discomfort. Fortunately, our team at Peninsula Osteopathy & Allied Health put together some information on common causes and types of overuse injuries, how we can assist you to address these injuries and how you can help yourself!
Overuse injuries typically develop gradually and can affect anyone engaged in repetitive activities. Some common causes include:
- Repetitive Motion: Repeatedly performing the same movements, such as running, jumping, or throwing, can strain the involved muscles, tendons, and joints.
- Training Errors: Increasing exercise intensity, duration, or frequency too rapidly without allowing adequate time for recovery can overload the body, leading to injuries.
- Poor Technique: Incorrect posture, improper form, or flawed biomechanics during physical activities can place undue stress on certain body parts, making them susceptible to overuse injuries.
- Inadequate Rest and Recovery: Failing to incorporate rest days into your exercise routine can prevent your body from healing and repairing itself, increasing the risk of overuse injuries.
Common types of overuse injuries include:
- Tennis/Golfer’s Elbow: Characterised by pain and inflammation/irritation in the tendons of the elbow, typically caused by repetitive wrist and forearm movements.
- Runner’s Knee (Patellofemoral Pain Syndrome): A common knee condition resulting from excessive stress on the kneecap, causing pain during running or activities involving knee bending.
- Shin Splints: Pain along the shinbone (tibia) caused by inflammation of the muscles, tendons, and bone tissue due to repetitive impact activities like running or jumping.
- Achilles Tendinitis: An inflammation of the Achilles tendon, the large tendon at the back of the ankle, caused by repetitive strain or overuse.

Here at POAH, our osteopaths can play crucial roles in the diagnosis, treatment, and rehabilitation of overuse injuries. We are able to assist you with:
- Accurate Diagnosis: We will conduct a thorough assessment to identify the specific cause of your overuse injury and determine the best course of treatment.
- Individualised Treatment Plans: Based on your diagnosis, we will develop personalised treatment plans incorporating a range of techniques such as manual therapy, exercise prescription, stretching, and strengthening exercises.
- Rehabilitation and Exercise Programs: We can guide you through progressive exercise programs aimed at restoring strength, flexibility, and function, while ensuring you regain optimal movement patterns.
- Education and Prevention: Finally we can provide valuable guidance on proper technique, training modifications, and injury prevention strategies to reduce the likelihood of recurring overuse injuries.
While professional guidance is crucial, self-management also plays an important role in the recovery process. Here are some practical tips for managing overuse injuries:
- Rest and Recovery: Allow your body sufficient time to rest and heal. Modify or temporarily halt activities that exacerbate your symptoms.
- Pain Management: Ice and heat pack strategies can be effective pain relievers, often personal preference dictates whether hot or cold will benefit you more. Over-the-counter pain relievers or anti-inflammatory medications, used under medical guidance, can also help manage pain and inflammation. Please ensure you consult with your medical practitioner to determine what is the most appropriate for you.
- Proper Technique and Form: Pay attention to your body mechanics and ensure you are using correct posture and technique during activities to reduce unnecessary strain on vulnerable areas.
- Gradual Return to Activity: When your symptoms improve, gradually reintroduce activities, starting with low impact and gradually increasing intensity and duration.
- Cross-training: Engage in alternative activities that work different muscle groups, reducing the repetitive strain on the injured area while maintaining overall fitness.
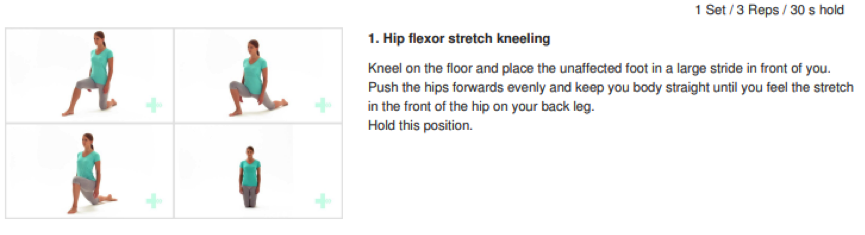
- Stretching and Strengthening: Perform specific stretches and exercises recommended by our team to enhance flexibility and strengthen the affected area.
Overuse injuries may try to slow you down, but they won’t stop you! Your passion for the activities you love is worth preserving, and your well-being matters. That’s why the team at Peninsula Osteopathy & Allied Health is here, ready to be your allies in recovery and vitality.
Don’t let pain hold you back. With our expert care and your commitment to self-management, we’ll help you reclaim your active, pain-free lifestyle. Remember, the sooner you act, the faster you’ll thrive. Reach out to us today and let’s conquer those overuse injuries together. Your journey to a healthier, happier you starts now!




 Osteoarthritis Management
Osteoarthritis Management