3 Tips to Get You Started on Your Running Journey
The coronavirus pandemic of 2020 has changed our lives dramatically. It has stopped us from seeing friends and family, made us change our hygiene habits (maybe for the better?) and significantly changed our routines and day-to-day existence.
With gyms closed and outdoor activities limited, I wanted a easy, quick and affordable way to fit exercise into my day.
And so like that, I took up running!
Now I am no expert, that is one thing I am sure of, but I can definitely impart some tips and tricks that I have put in place to keep me motivated and committed to the cause, because to be honest, running in itself is pretty boring.
What keeps me coming back is the post-run endorphin hit that you get with any exercise, what a great way to start the day!
For all the beginner runners out there, this is what I have incorporated to keep me going.
Set Goals
Probably the easiest and most effective tip towards achieving your goals is to create them in the first place! Too many times I have seen clients and patients (and of course me personally!) start exercise classes or rehabilitation programs with vague and ambiguous end points.
“Get fit”, “get stronger”, “improve flexibility”, “increase my core strength” are some common ones that get bandied around. The problem with these is that they aren’t specific enough.
One great way to create clarity with goal setting is to use the S.M.A.R.T acronym. SMART goals are specific, measurable, achievable, relevant and time-orientated. If we take running as our example to create a SMART goal, it might look something like this:
I want to run 21kms continuously, by the start of next year (6months time).
This goal is specific (21kms continuously), it is measurable (we can track progress via measuring Km’s ran), it is achievable (yours may be different based off your level of fitness/experience), it is relevant and has a date attached to it. From this we can work backwards and put a plan in place to reach this goal.
Track your progress
There is now an abundance of ways that we can do this with modern technology – from phone apps all the way up to top of the range wearable watches. If you are a beginner like me, using a phone app would be the best place to start. I have been using the RunKeeper app from Asics. It’s free and has all the features needed to give you the right amount of information and feedback.
Measuring and tracking your progress over time creates buy-in, tells you how you are tracking towards your goals and can create that little extra bit of incentive to stay with the process when the last thing you feel like doing is going out and exercising.
On the flip side, try not to get too bogged down on the day-to-day progress and running times/splits/Km’s ran. Being sick, tired, fatigued from work, dehydrated, stressed etc. are all factors that can influence your run. As long as the overall trend is a positive one, it’s ok to feel crappy from time to time.
Injury Prevention – Warm-up, work on your weaknesses & manage loads
Avoiding any significant disruptions or prolonged time-off from running is going give you the best chance at reaching your goals. As an Osteopath, I could write a whole blog post on this topic alone! (Maybe I will?).
Injury prevention doesn’t mean spending every other day in the gym or getting weekly massages – as nice as that may be!
There are a few simple strategies that you can do to limit your chance of getting hurt:
Warm-up
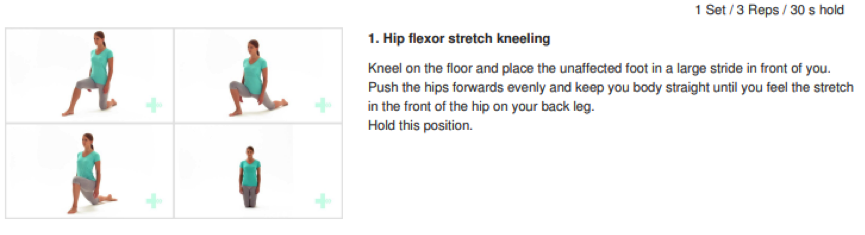
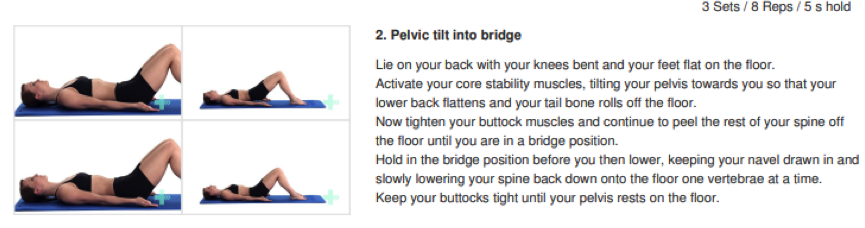
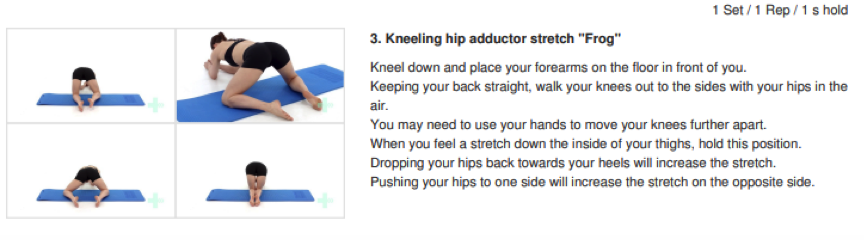
A 5-10minute warm-up prior to going for your run may help to limit the chance of an injury occurring in the first place or speed-up your recovery post-run. Your warm-up should consist of some flexibility-based and strength-based movements that target all the parts of the body that you will be using during the run. Common stretches and exercises in a warm include dynamic stretching (think leg swings, trunk twists etc.), strength-based exercises (squats, lunges, single leg exercises) and neuromuscular exercises (high knees, butt flicks, grapevines etc.).
Make your legs and trunk resilient and adaptable
Another way to prevent injuries from slowing you down is to build your bodies capacity to be resilient against running, this can be done by increasing the strength in your leg and trunk muscles. Going through a systematic and thorough musculoskeletal assessment with your trusted health professional will help identify areas of weakness and then will allow you to put in place strategies to adjust accordingly. At Peninsula Osteopathy & Allied Health, a common running assessment may include things like testing the range-of-motion and strength in your ankles, knees, hips and spine. From this we can then give you exercises and hands-on treatment to improve these deficits.
Manage your loads
I.e don’t do too much but don’t do too little. Maybe the biggest cause of injuries in any training program is increasing your loads too quickly. This is because your body doesn’t have the capacity to deal with the loads and stresses you are putting it under. Again, another topic that we could dive deeply into with various guidelines and protocols, but for beginner runners (like me) splitting your running program into 2 week blocks and not increasing your overall running load by more than approximately 10% each block can limit the chance of any flare-ups. A multitude of factors can contribute to overall ‘load’; running distance, speed, elevation and amount of rest can all be altered to make runs easier or more difficult. Tracking your progress via an app or watch gives you more data to make informed decisions and prevent any excessive fluctuations in load.
Should you have any questions or wish to know more about a warm-up or how to reduce your chance of injury during running, give the clinic a call to speak to one of our experienced Osteopaths, Myotherapists or Exercise Physiologists on 5253 2345.